Today we feature a new article from, JD Moyer of the blog Systems for Living Well:
Recently a few articles and studies have come to my attention that have expanded my understanding of vitamin D metabolism, and raised a few questions as well. As previous posts on this blog have advocated relatively high doses of vitamin D3 supplementation for various conditions (especially asthma), I think it’s my responsibility to consider and address this new information.
Most notably:
1. A study out of the Netherlands has identified genetic variants that are associated with both low levels of 25-hydroxyvitamin D and increased longevity. This is the opposite finding of what we might expect from many studies that link higher vitamin D to lower levels of disease. So what to make of it?
2. Paul Albert and Amy Proal discuss why they think vitamin D supplements are mostly harmful in this post. If I correctly understand their main argument, they think that vitamin D may have a short-term palliative effect by suppressing immune response and reducing inflammation, but may have long-term negative health effects by allowing chronic bacterial and viral infections to grow and spread in the body.
3. Todd Becker discusses why he doesn’t take vitamin D supplements in this post. He references Albert and Proal’s research, and suggests that vitamin D sensitivity might be downregulated by excessive supplementation. He notes that the biologically active form of vitamin D (1,25-dihydroxyvitamin D3, or calcitriol) is produced from 25-hydroxyvitamin D by the kidneys, but that most tests only measure 25-hydroxyvitamin D. Some people have low levels of 25-hydroxyvitamin D but adequate or even high levels of calcitriol (the biologically active form of vitamin D).
The Marshall Protocol
Here’s my favorite quote from Albert and Proal’s post re: questioning the consensus on vitamin D:
We suspect that people would be less willing to take extremely large amounts of vitamin D if they were actually told, “We’re giving you high doses of a secosteroid that will adjust your hormonal and immune activity in ways not yet fully understood.”
I completely agree! Any concentrated substance we put into our bodies might end up doing more harm than good. We should be cautious, and always use the minimum effective dose.
But reading further, I learned that Proal and Albert are advocates of the Marshall protocol. The Marshall protocol suggests that certain autoimmune diseases, including sarcoidosis, rheumatoid arthritis, fibromyalgia, and many others, can be cured by lowering vitamin D levels (by avoiding sunlight, food sources, and supplements), taking rounds of low-dose antibiotics, and taking a drug called Benicar.
Trevor Marshall is a former electronic synthesizer designer and custom amp builder for AC/DC. What an interesting guy! At some point Marshall was diagnosed with sarcoidosis, an inflammatory autoimmune disease. He eventually developed the Marshall protocol, and founded the Autoimmunity Research Foundation.
The hypothesis behind the Marshall protocol is that most chronic diseases are the result of chronic bacterial infections, wherein invading bacteria lose their cells walls and congregate into biofilms, thus becoming resistant to both antibiotics and the body’s own immune system (as well as detection by most medical tests).
According to Marshall, these biofilm “L-form” bacterial colonies produce metabolites which bind to vitamin D receptors (VDRs). This interferes with the production of antimicrobial peptides (AMPs), and important part of our immune system that helps destroy bacteria, viruses, and fungi.
Albert and Proal have published a study that suggests that in some people with autoimmune disease, levels of 1,25-dihydroxyvitamin D3 (the biologically active form of vitamin D produced by the kidneys) are elevated, while levels of 25-hydroxyvitamin D (measured by most vitamin D blood tests) are low. They hypothesize that low vitamin D levels are caused by chronic disease, rather than being a predictor of disease.
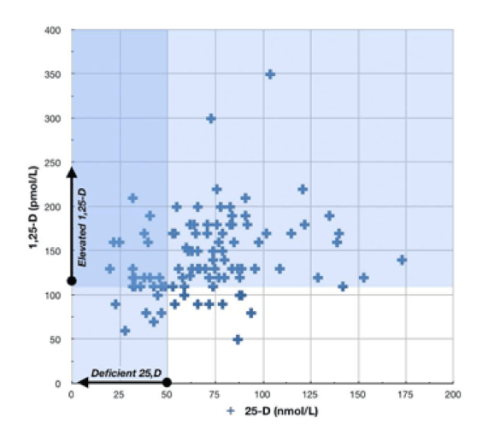
Vitamin D levels from Blaney/Albert/Proal’s study.
What to make of this? This is the same graph used by Todd Becker in his post re: why he doesn’t take vitamin D supplements, to support his assertion that biologically active vitamin D (1,25-D) isn’t necessarily correlated with tested vitamin D levels (25-D). What Becker doesn’t mention is that this graph represents only people with autoimmune diseases (like sarcoidosis). And if you look at it, you can see that mostly 25-D and 1.25-D are correlated … there are just a few exceptions in the dark blue area.
Is there an alternate hypothesis to explain why vitamin D might worsen sarcoidosis, and possibly other autoimmune diseases? Yes there is. Enter Dr. John Cannell (excerpted from this post):
Furthermore, it is well known that sunlight can cause high blood calcium in patients with sarcoidosis. In fact, sarcoidosis is one of several granulomatous diseases with vitamin D hypersensitivity where the body loses its ability to regulate activated vitamin D production, causing hypercalcemia.
By “loses its ability to regulate activated vitamin D production,” Cannell is referring to the body making too much 1,25-dihydroxyvitamin D3 from 25-hydroxyvitamin D (in the graph, the people in the “elevated 1,25-D” section).
Whatever the reason, it does seem to make sense for people with sarcoidosis, and possibly other autoimmune diseases, to experiment with lowering vitamin D levels. But there may be dangers to implementing the Marshall protocol. Again, from Cannell:
However, if Dr. Marshall’s principal hypothesis is correct, that low vitamin D levels are the result of disease, then he is saying that cancer causes low vitamin D levels, not the other way around. The problem is that Professor Joanne Lappe directly disproved that theory in a randomized controlled trial when she found that baseline vitamin D levels were strong and independent predictors of who would get cancer in the future. The lower your levels, the higher the risk. Furthermore, increasing baseline levels from 31 to 38 ng/ml (77.5 to 95 nmol/L) reduced incident cancers by more than 60% over a four year period. Therefore, advising patients to become vitamin D deficient, as the Marshall protocol clearly does, will cause some patients to die from cancer.
As you can imagine, Marshall has some problems with Lappe’s research. But Cannell’s interpretation of the available data makes more sense to me.
Here’s another post on the Marshall protocol worth reading.
What About Asthma?
I take up to 20,000IU of vitamin D a week. Taking supplemental vitamin D, along with a mostly paleo diet, keeps me free of asthma symptoms.
Why does vitamin D help asthma?
Is vitamin D actually an immunosuppressant? That would line up with Marshall’s ideas. Maybe vitamin D works by somehow calming down the immune system and making it less reactive or “twitchy.” Proal calls vitamin D a “pallative” and predicts that that anti-inflammatory effects we see from supplemental vitamin D will be followed up by longer-term damage (decades later) from chronic bacterial infections.
But vitamin D can boost the immune system, for example fending off colds and influenza A. This makes sense — adequate vitamin D stimulates vitamin D receptors (VDRs) to produce adequate antimicrobial peptides (AMPs). According to Cannell, the AMPs working by poking holes in the lipoprotein coat that influenza A uses to protect itself. Some folks at MIT actually took pictures of the process!
I don’t know exactly why vitamin D helps asthma, and I’m not sure anyone does at this point. If you know of a good, detailed explanation, please add it in the comments.
Too Much Vitamin D
How much is too much? For myself, I’ve noticed excessive thirst, constipation, and less restful sleep from taking too much vitamin D — symptoms that quickly go away when I cut back. Magnesium can potentially ameliorate these symptoms, but I’ve noticed side effects even when taking vitamin D with magnesium glycinate (a highly absorbable form), and even when supplementing with other fat soluble vitamins (vitamin A and K2).
Some people notice negative effects on much lower doses than the ones I find to be therapeutic. Maybe this has to do with low magnesium, or maybe it has to do with higher conversion rate to the biologically active form of vitamin D by the kidneys.
If you are you in good health without taking vitamin D, and you notice negative effects from taking supplemental vitamin D, then either reduce the dose, or stop taking supplemental vitamin D altogether and just get what you need from regular sun exposure.
Note that washing your skin with soap after sun exposure can prevent the vitamin D precursor that forms on your skin from being absorbed into your bloodstream.
On the other hand, if you get a great deal of sun, don’t think that you’re safe from the possibility of getting too much vitamin D. Skin cancer risks aside, sunbathing has been linked to both worsening sarcoidosis [PDF] and kidney stones.
Just because it’s the “natural” way to get vitamin D doesn’t mean it’s totally safe. Plenty of natural things can kill you (like komodo dragons, and sun-worship).
The Heemst Study, and Klotho Protein
From digging deep into the raw data of my 23andMe.com profile, I know that I carry several variants that are associated with lower levels of vitamin D. Unfortunately, I don’t know how to interpret the raw data related to gene CYP2R1, which, according to the the recent Diana van Heemst study, is related to both low 25-hydroxyvitamin D levels, and longevity.
Van Heemst found that “the offspring of nonagenarians, people over the age of 90, with at least one nonagenarian sibling, had lower levels of vitamin D as well as a lower frequency of common genetic variants in the CYP2R1 gene.“
From the same article:
“We speculate that offspring might have a higher expression of the klotho protein, which is hypothesized to be an ‘aging suppressor’ protein,” van Heemst and her team wrote.
What do we know about klotho? In mice, klotho suppresses aging. In humans, klotho expression is related to levels of calcitriol. Specifically:
In humans, a specific genotype of Klotho has been found to be associated with lower Klotho gene expression and a decrease in survival of dialysis patients. The association was more pronounced among patients who were not treated with active forms of vitamin D. [study]
[Thank you to user "little bit" on the 23andme forum for the link]
So maybe the van Heemst nonagenarians express higher klotho, and thus more efficiently convert 25-D (from sunshine and supplemental D3) to 1,25-D (calcitriol, activated vitamin D)?
Equally possible is that I’ve misinterpreted the mechanisms described in the klotho article — feel free to comment if you think I’ve gotten it wrong. I’m not trained in medicine or biology!
I wonder if these “high klotho” folks are also vulnerable to hypercalcemia and/or autoimmune problems if they get too much sun, or take too much supplemental vitamin D.
Conclusion
Unfortunately I don’t have one … just more questions. My advice, if I were a doctor, would remain the same. If you suffer from asthma symptoms, try taking supplemental vitamin D3, up to 5000IU a day, along with magnesium, and see if that improves your condition. Going on some variation of the paleo diet (thus reducing systemic inflammation, reducing gut permeability, and modifying the composition of your gut biome) may also help you, as it helped me.
To this I would add — if you experience negative side effective from taking vitamin D3 along with a chelated form of magnesium (like citrate or glycinate) then reduce the dose of vitamin D and increase the magnesium, or just stop taking vitamin D altogether and get some sun.

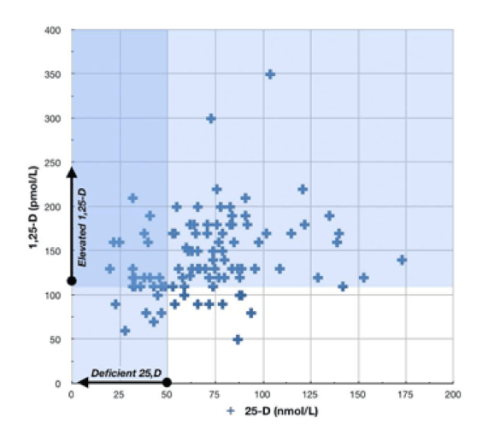 Vitamin D levels from Blaney/Albert/Proal’s study.
Vitamin D levels from Blaney/Albert/Proal’s study.